You may already know about our patient portal, but do you know about all the benefits of using it?
The Georgetown Pediatrics Patient Portal is a secure way to check on your child’s health records and even download and print them for school, sports, or your home records. You don’t have to be a computer genius or internet guru to use the site. It’s now more user-friendly than ever, so if you haven’t checked it out in a while, we hope you’ll do so soon.
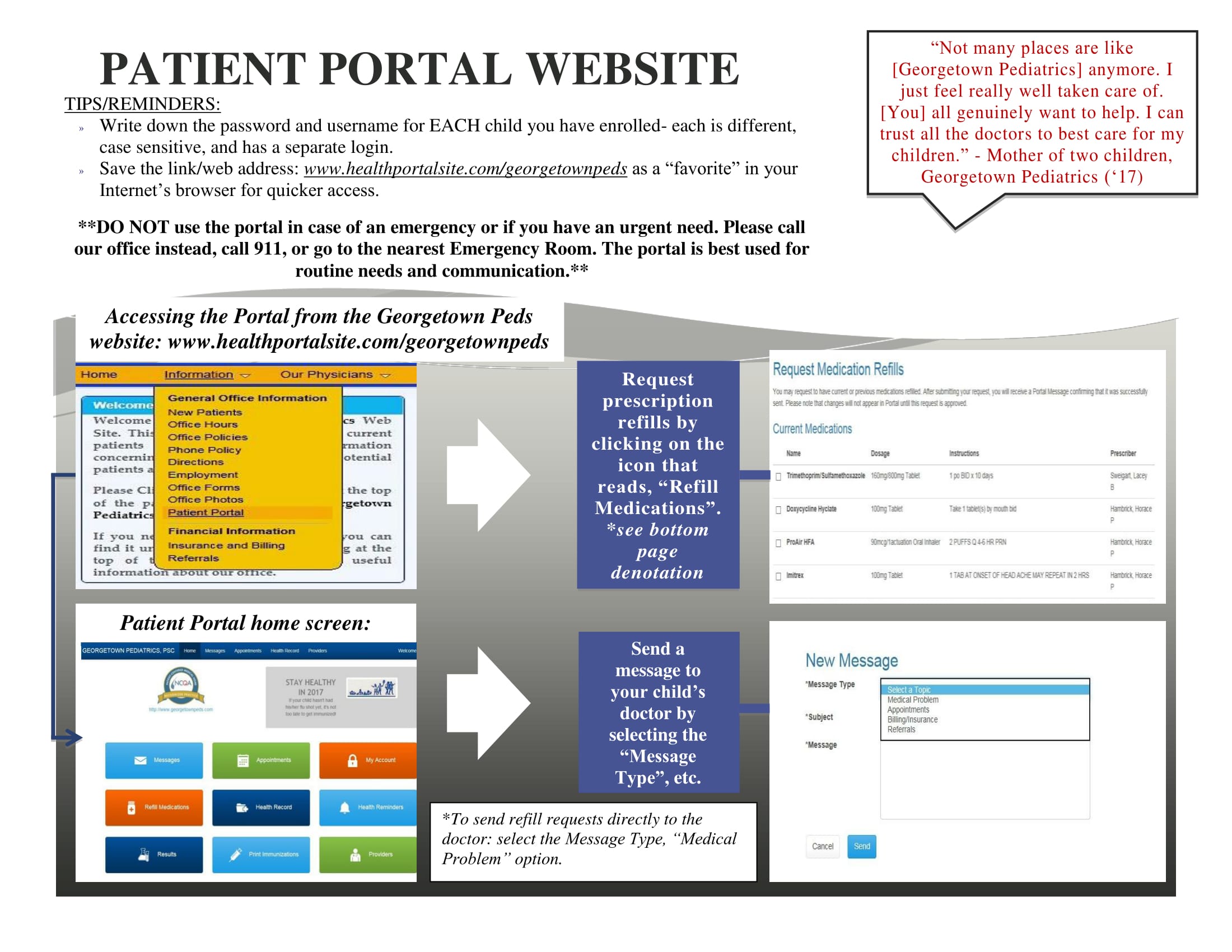
If you haven’t registered (or don’t remember if you have or not), make sure we have your current email address. Then go to the portal’s website, www.healthportalsite.com/georgetownpeds, to sign in. You’ll need a separate password and username for each child, so be sure to record them somewhere in a secure place.
How and why might you use the portal? Here are a few things you can do easily on your child’s portal page:
- verify appointments;
- view and print immunization records;
- receive documentation from our office (school notes, medication forms, FMLA forms, etc.);
- direct communication with your child’s physician;
- refill medications;
- see a list of all medications;
- view lab and diagnostic results;
- update personal information (address, phone number, emergency contact).
As you can see, the convenience of the patient portal is a great addition to your busy life.
Our brochure with more information is attached. Please take a few moments to look it over and start accessing your child’s medical information anytime, anywhere from your computer or smart phone.